Pitfalls in Diagnosis
Every year children are sent home from hospital with undiagnosed meningococcal disease. This leads to wasted hours in which the disease progresses and children may die unnecessarily. Simple changes to clinical practice may help prevent this. Common pitfalls in practice are explained in this section.
Contacts of cases of meningococcal disease

After a case of meningococcal disease, there is an increased
risk for school and nursery contacts
People who have been in contact with cases of meningococcal disease are at increased risk of invasive disease. After a single case, close household contacts-usually family-are at the greatest risk, but there is an increased risk for school contacts as well37.
12 year old boy presented with a short history of fever, dizzy and nauseated. A member of his class was then on intensive care with meningitis. His mother was concerned that he might have the same illness.
On examination he was febrile, temp 38.5, alert and orientated.
He was assessed by a doctor who found that he was alert, with no neck stiffness or photophobia. He did not have a rash and his chest was clear. The doctor diagnosed a viral illness and sent him home.
He returned 12 hours later with fulminant septicaemia and died.
Guidelines for the public health management of meningococcal disease are based on the statistical probability of further cases occurring and the risk/benefit balance of control measures that can be taken38. Wider public health action only comes into play after two or more linked cases. Although the great majority of cases of meningococcal disease are sporadic and do not result in further linked cases, clusters of cases do occur. When assessing a child whose classmate has meningococcal disease, consider that this could be the second case that makes the cluster.
Diagnosing "meningitis"
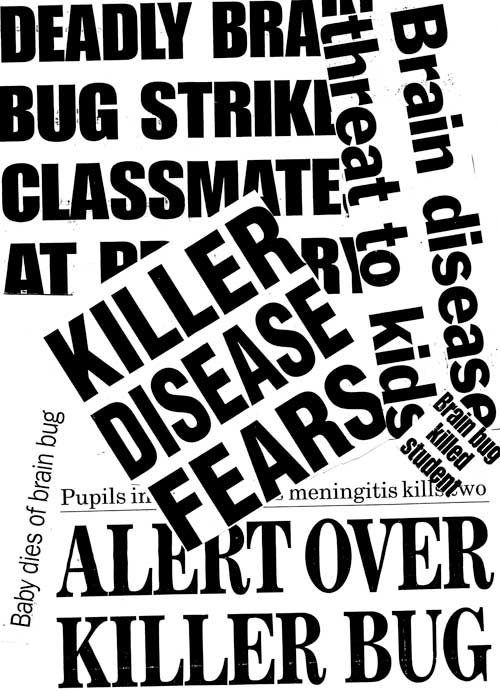
'Deadly brain bug' - the media portray meningococcal disease as meningitis even when the subject is a case of meningococcal septicaemia
Parents are usually not aware that there is a difference between meningitis and septicaemia and it is up to doctors to ask about the symptoms of sepsis and ensure that their clinical examination includes looking for shock.
Making a provisional diagnosis.

A diagnosis based only on symptoms should be viewed as changeable until you have confirmation from investigations.
When giving a child a presumptive diagnosis like 'febrile convulsion' or 'viral illness' remember that it is just that-your best guess.
2 year old admitted with a history of fever, cough, fast breathing and fast pulse noted by the mother.
The child had experienced a 10 minute generalised convulsion at home.
On admission the child had a fever of 39.3, Pulse 220 bpm, RR 35/min, saturations 99 and no rash noted.
A diagnosis of febrile convulsion was made and the child was admitted to the ward.
1 hour after admission the pulse was fast at 186, BP 95/50 and respiratory rate 50. No investigations were sent.
2 hours after admission the child had a second fit for a few minutes. The medical staff decided that this was just a second febrile convulsion and did not change management or investigate. The persistent tachycardia and tachypnoea were not taken into consideration.
During the next 5 hours on the ward there were no recorded vital signs at all. Then the child was noted to have extending purpura and to be shocked. Full resuscitation was started but it was too late and the child died.
How much rash do you need to diagnose meningococcal disease?

A few petechiae on mottled skin Especially in the early stages, or when meningitis predominates, rash may be scanty, blanching or even absent.
Remember that the process of meningitis or septicaemia can be quite advanced before the rash starts to appear, so if you suspect that a child may have meningococcal disease then do not wait for more rash to develop, treat the child immediately.
2 year old boy seen by the GP: acutely unwell with high temp, vomiting, lethargy, unable to keep fluids down. Extra concern - close contact has been diagnosed as having Meningococcal Meningitis
GP examination fever 38.6, pale, no rash, tachycardic but not shocked, irritable on handling.
Seen in hospital: Pale and quiet Temp 39.6, P 155, RR 58 , No rash, thirsty
Given paracetamol, vomited immediately
SHO examination: Very lethargic, sleepy but rousable, Pale
RR 60, P140, No neck stiffness, 2 petechiae in nappy area
Diagnosis ? viral illness
Reviewed by registrar: diagnosis - this was likely to be a viral illness and to admit for observations, to have antibiotics if more rash appeared.
12 hours later- consultant ward round- looking worse with more rash. Investigations initiated.
Hb 10 , WCC 22.5 , Pl 244
pH 7.29 , pCO2 4.39, pO2 4.6, BE -10
INR 2.0 , APTR 1.3
Child deteriorated quickly at this point and died
Other rashes.
If you diagnose a child as having another illness characterised by a rash, make sure that your diagnosis is likely or even possible.
You may be sure of your diagnosis, but if you decide the child is well enough to be sent home, remember to advise parents to return if their child becomes more unwell, even if this is only shortly after being seen.
Teenagers

Approximately 25% of teenagers carry meningococci in the nasopharynx
Teenagers are a vulnerable group. There is a secondary peak in incidence of meningococcal disease amongst young adults aged 15-20 years, with an increased risk of mortality39.
As shown in this learning tool, in the section Development of Symptoms in Meningococcal Disease, signs and symptoms develop later in teenagers than in younger children. Teenagers present to GPs and to hospital later than younger children do, and on average the disease is further advanced in teenagers by the time they get to hospital.
He walked into ED - no rash, alert and orientated. HR 160, RR20, Temp 39, BP80/40, saturations 96% in air.
After 30 minutes he developed rapidly spreading purpura.
Hb 13.7, WCC 1.4, platelets 9.
Na 134, K 3.2, Urea 6.2, creat 163
PH 7.1, pCO2 4.9, pO2 4.1, BE -13.8
He was resuscitated aggressively but died.
Does your diagnosis make sense?

Assessing febrile children and trying to decide what is wrong with them is one of the most difficult tasks in paediatrics
It takes time to take a good history and examine a child properly. Before you discharge the patient from your care make sure that what you have done makes sense and that you can explain your actions and decisions to anyone who may ask.