Background to Disease
back to top^Disease burden
Meningococcal disease can kill in hours and takes more than one hundred lives in the UK each year8. It is not only associated with a significant risk of mortality, but also with long term morbidity. Those who recover may be left with disabilities that dramatically alter their lives, including amputations, scarring, sensory deficits, intellectual impairment, epilepsy, and a range of less specific cognitive and psychological disorders. The meningococcus is the main cause of bacterial meningitis in children and young adults, and a common cause of septicaemia and shock at these ages. Cases of meningococcal disease reached a 50-year peak in 1999. That year MenC vaccine was introduced and has had a tremendous impact. Cases of serogroup C meningococcal disease have dropped by over 90%9. However, serogroup B meningococcal disease was more common, particularly in children, even before MenC vaccine was introduced. No vaccine available can protect against most group B serotypes and sero-subtypes circulating in the UK, so serogroup B disease continues to fluctuate unchecked.
Lab-confirmed meningococcal disease, children and adults, England and Wales9
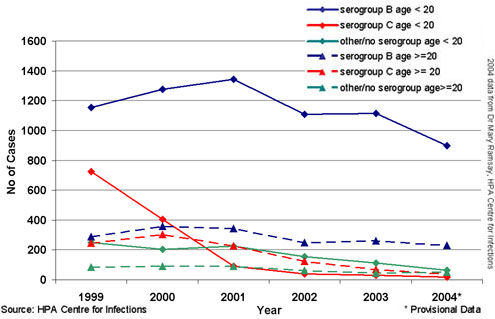
Based on lab-confirmed cases, the incidence of meningococcal disease in England and Wales in 2004 was 7.5 cases per 100,000 population aged less than 20. Enhanced Surveillance of Meningococcal Disease aims at more complete ascertainment of cases, and in 2004, identified approximately half again as many cases as were laboratory confirmed. Enhanced Surveillance currently reports10 that the rate of confirmed meningococcal disease is highest in the under-fives, particularly among infants: 52.9 cases per 100,000 < 1 year of age, 18.8 cases per 100,000 aged 1-4 years. In children older than 4 years of age, the rate is 3.1 cases per 100,000. Case fatality ratios in children are highest in teenagers older than 14, followed by infants less than 1 year of age.
Cases of meningococcal disease were lower in 2004 than for many years, but for 2005, the Meningococcal Reference Unit reports an increase of 11% from the previous year11. These figures are for England and Wales, but incidence rates are similar across the UK.
back to top^Characteristics of meningococcal disease
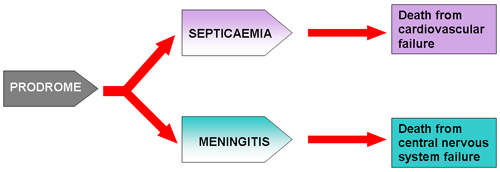
The two major clinical forms of meningococcal disease are meningitis and septicaemia. Most patients will have a mixed presentation. A minority will have pure septicaemia and it is these patients who carry the worst prognosis and maximum effort must be made to identify them early12. There are important differences in the pathophysiology of meningitis and septicaemia which underlie the clinical presentation and management of the two main forms of the condition (see pathophysiology).
back to top^Disease pathway
back to top^Clinical features of severe disease
The diagram above illustrates the main causes of death from MD. In the majority of patients, one disease process predominates. Patients presenting with mixed disease will also tend, as the disease worsens, to become either profoundly septicaemic or profoundly meningitic. A few will have combined severe septicaemia with shock and severe meningitis with raised intracranial pressure and these need expert management. Patients presenting with septic shock without meningitis carry the worst prognosis8 13. Although a few patients with meningitis will die from raised intracranial pressure, most deaths from MD result from shock and multi-organ failure14.

back to top^Features which predict poor prognosis at the time of presentation include13 14
- Presence of shock
- Absence of meningism
- Rapidly progressive purpuric rash
- Low peripheral white blood cell count
- Thrombocytopenia
- Markedly deranged coagulation
- Depressed conscious level











