Principles of Management
Management of septicaemia and meningitis
The aim of this section is to outline the principles of management of septicaemia and meningitis which are based on understanding the pathophysiology. A fuller explanation of the management of meningococcal disease can be found in Archives of Disease in Childhood 5. The protocol from this article has been published as ‘Early Management of Meningococcal Disease in Children’ and is accessible from the next button on the menu bar at the top of the page. It is also available as a leaflet or poster from Meningitis Research Foundation.
Antibiotics - Cefotaxime or ceftriaxone
- All children with fever and a haemorrhagic rash
- Children with shock with or without a rash
- Children with clinical evidence of meningitis. If lumbar puncture is contraindicated, treat immediately with antibiotics and lumbar puncture when safe (but full set of bloods as well as throat swabs for culture should be taken if not already done). Consider adjunctive dexamethasone before, with or within 4 hours of the first dose of antibiotics, if there are no signs of septic shock42
Door to needle time
43Once the decision to give antibiotics has been taken, ensure they are written up and given within 30 minutes. Unacceptable delays in giving antibiotics can occur when responsibility for this is delegated without personal follow up.
Principles of management of septicaemia with shock
This section provides a narrative description of the management plan outlined in the protocol Early Management of Meningococcal Disease in Children .
Children with evidence of shock need immediate resuscitation:
- Assess airway for patency
- Give oxygen to all patients even if oxygen saturations are normal in order to optimise tissue oxygenation
- Secure good venous access. The goal of circulatory support in shock is the maintenance of tissue perfusion and oxygenation. Remember in shocked children the intra-osseous route may be the most effective way of giving large volume replacement.
- Rapid fluid resuscitation should be initiated. Boluses of 20ml/kg of colloid (preferably 4.5% albumin44) or crystalloid solutions should be given rapidly (over 5-10 minutes) whilst monitoring the clinical response (HR, RR, BP, CRT, O2 sats, urine output, conscious level). If the clinical response is short-lived or absent, and shock does not improve or progresses, large volumes may be required (over 60ml/kg in the first hour).

Bloated appearance due to capillary leak syndrome. Fluids given during volume resuscitation contribute to this at first.
There is evidence from adults that early goal-directed resuscitation of patients with septic shock is associated with an improvement in outcome45. - Hypoglycaemia (<3.3 mmol/l) is common and should be corrected: 5ml/kg 10% dextrose bolus i.v., then check glucose hourly and correct if necessary.
- If signs of shock persist after 40-60 ml/kg of fluid resuscitation, there is significant risk of pulmonary oedema, so elective tracheal intubation and mechanical ventilation should be initiated even if there are no signs of respiratory failure3. This will optimise oxygenation, reduce the work of breathing, and improve cardiac function.
- Advice to guide further management should be sought early.
- Invasive monitoring and central venous access will be required to guide fluid therapy and optimise support.
- Inotropic support may be required to optimise tissue perfusion and improve myocardial function.
- Metabolic acidosis is common and impairs myocardial contractility. If pH<7.2 due to base deficit, give half correction NaHCO3 iv.
- Volume (ml) to give = (0.3 x weight in kg x base deficit ÷2) of 8.4%NaHCO3 over 20 mins.
- In neonates, volume (ml) to give = (0.3 x weight in kg x base deficit) of 4.2% NaHCO3.
- Metabolic derangements of calcium, magnesium and potassium are common, and need frequent checking and correction .
- In cases of severe bleeding or profound clotting disorder, consider correction of coagulopathy with fresh frozen plasma, platelets and, if fibrinogen is low, cryoprecipitate. Correction of thrombocytopaenia is not generally required, but if uncontrolled haemorrhage from venepuncture sites or mucous membranes occurs despite replacement of clotting factors, platelet transfusion may be required if platelets are below 50,000/mm3.
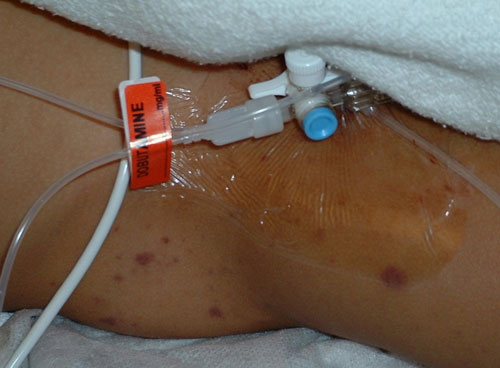
Dobutamine can be infused centrally or peripherally
Remember – Call for senior help early. Sick septic children need experienced doctors. This is not the time to ‘have a go!’
Principles of management of meningitis with raised intracranial pressure
The main objective in managing patients with RICP is to maintain oxygen and nutrient delivery to the brain. Call for senior help and Paediatric Intensive Care immediately if there are signs of RICP.
- Patients with GCS < 8 or drop of 3 points in last hour, or fluctuating level of consciousness should have their airway secured by tracheal intubation and mechanical ventilation.
- Optimise ventilation to ensure normocapnia and avoid hypoxia. Cautious fluid resuscitation. Maintenance of circulating volume and adequate blood pressure is the goal. Overaggressive fluid resuscitation will exacerbate cerebral oedema. Only patients with shock require aggressive fluid resuscitation to ensure cerebral perfusion. Patients without shock require close monitoring and judicious fluid replacement depending on heart rate, blood pressure, urine output and metabolic acidosis.
Do not rely on capillary refill time to guide fluid management as this may be falsely prolonged in patients with raised ICP. Rely instead on the other markers of organ perfusion and circulatory status as described.
Consider the use of mannitol or hypertonic saline for acute changes in ICP as suggested by pupillary changes or sudden onset hypertension and bradycardia.
Nurse patient in head-up position, 20-30 degrees from horizontal. Avoid inserting central venous lines into the internal jugular vein as this impedes venous drainage of the head and the insertion of the line may exacerbate the raised intracranial pressure.
Public health
- Doctor immediately notifies any suspected case of meningitis or meningococcal septicaemia by phone to the Consultant in Communicable Disease Control (CCDC), Consultant in Public Health Medicine (in Scotland) or on-call Public Health Specialist. This is the legal duty of the doctor who makes or suspects the diagnosis – usually the hospital doctor notifies even if the case was referred by a GP.
- After a single confirmed or probable (i.e. where MD is the most likely clinical diagnosis) case of meningococcal disease, only close contacts living in the same household as the case in the 7 days before disease onset, or kissing contacts need antibiotic prophylaxis38.
- Healthcare staff only require prophylaxis if their mouth or nose has been splattered (clearly felt) with large particle droplets/secretions from the respiratory tract of a patient with confirmed or probable meningococcal disease, or if conjunctivitis develops within 10 days of exposure 46. This is unlikely to occur except when using suction during airway management, inserting an oro/nasopharyngeal airway, intubating, or if the patient coughs in your face.
- Public Health, usually the CCDC/CPHM arranges for prophylactic antibiotics to be prescribed to contacts as necessary. Rifampicin, ciprofloxacin (not in children under 2 or in pregnancy), and ceftriaxone (by injection) are all recommended for use in preventing secondary cases of meningococcal disease, but only rifampicin is licensed for this purpose. Rifampicin interferes with the oral contraceptive pill and stains body fluids red, including urine and saliva, and permanently stains soft contact lenses. Some individuals may experience rash or stomach upset.
- Antibiotic prophylaxis should eliminate carriage, but if the contact is already incubating the bacteria, he or she can still get the disease. Close contacts of a case need to understand that they are at increased risk of meningitis and septicaemia, and should be alerted to the symptoms, and given a leaflet on meningitis and septicaemia.
- The CCDC/CPHM will:
- arrange for the next of kin to be interviewed to establish other close contacts and will arrange prophylaxis for them, and for later immunisation of all close contacts if indicated
- ensure information is disseminated to appropriate local schools, work places and general practitioners
- be responsible for early detection of clusters and outbreaks of disease.











