Pathophysiology
Understanding the pathophysiology of meningococcal infection and the principles of management
The principles of management of meningitis and septicaemia are best understood by having a basic knowledge of their pathophysiology40.
The section below is a summary. For more detailed information see references section.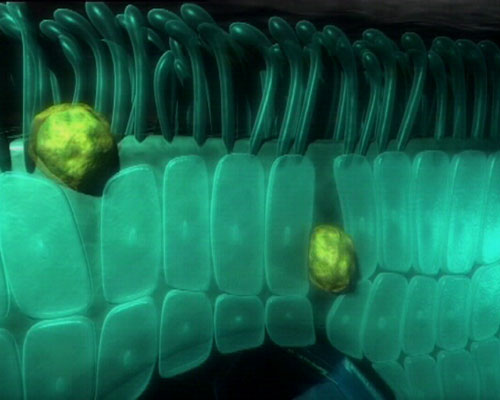
Clinical pathophysiology of meningococcal septicaemia
back to top^Increased Vascular Permeability
When meningococci invade the bloodstream, endotoxin is released from the bacteria. This triggers an inflammatory response, with release of inflammatory mediators, which is directed against the endothelial surface lining the blood vessels. One of the main functions of the endothelium is regulation of vascular permeability, and disturbance of this function causes the endothelial lining to become 'leaky', allowing increased passage of protein and water from the intravascular to extra-vascular compartments, causing a 'capillary leak syndrome'. The patient becomes hypovolaemic due to reduction in circulating volume, thus reducing cardiac output.
In compensation for reduced circulating volume, heart rate and contractility increase, and perfusion to skin and the splanchnic circulation is reduced. Therefore signs of hypovolaemia in sepsis include:
- Tachycardia
- Tachypnoea
- Cool peripheries
- Reduced urine output
- Irritability or lethargy.
Note that in the early phases of septic shock blood pressure is maintained by these compensatory mechanisms. This means that early in shock, children are alert as blood flow to the brain is being maintained at the cost of the other organs.
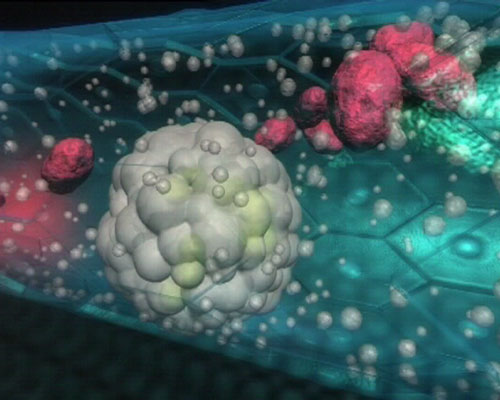
back to top^Myocardial dysfunction
Endotoxin and inflammatory mediators (such as IL6)41, together with other poorly defined 'myocardial depressant factors' reduce myocardial contractility. In addition, a myocardial cytotoxic process causes myocardial cell necrosis.
Hypovolaemia and myocardial dysfunction contribute to progression of shock. In addition, nitric oxide and other vasoactive mediators cause a relative 'vasoparesis' and relative inotrope unresponsiveness.
Progression of shock leads to tissue hypoxia and capillary leak leads to pulmonary oedema resulting in tachypnoea and hypoxia.
Eventually, compensatory mechanisms fail and blood pressure falls. This is a late and serious sign in septic shock in children.
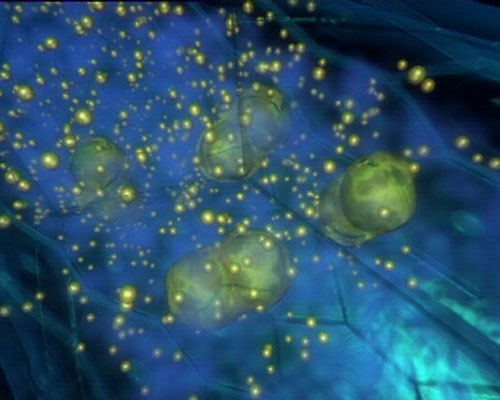
back to top^Disseminated intravascular coagulation

Endotoxin and the inflammatory response leads to activation of the coagulation cascade and down-regulation of anticoagulant and fibrinolytic pathways, leading to a procoagulant state. Clotting times are prolonged and thrombocytopenia occurs.
Microvascular thrombosis contributes to multiple organ failure and purpura fulminans.
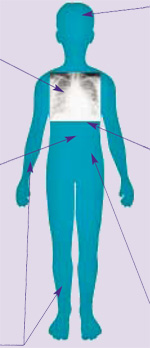
Amputations:
When purpura fulminans occurs, some tissues are irreversibly destroyed due to thrombosis within the microvasculature, combined with vasoconstriction and ischaemia in peripheries. Haemorrhagic necrosis in skin and clotting in small vessels can lead to loss of skin, digits or limbs.
Specific organ dysfunction in shock
| Respiratory failure (arterial PO2 <10kPa in air or PCO2 >6) Common in shock. Capillary leak into lung parenchyma  acute pulmonary oedema. Clinically: tachypnoea, chest wall retraction, hypoxia. acute pulmonary oedema. Clinically: tachypnoea, chest wall retraction, hypoxia. |
 |
|
Metabolic derangement Septicaemia causes profound acidosis and derangements in metabolism, which may affect myocardial function and need correcting. Hypoglycaemia is common. Hypokalaemia, hypocalcaemia, hypomagnesaemia and hypophosphataemia all occur. |
Myocardial failure
Depressed myocardial function is multifactorial, including endotoxin, cytokines, multiple metabolic derangements, hypoxia, and hypovolaemia. Clinically: tachycardia, gallop rhythm, cool peripheries and eventually hypotension. |
|
Coagulopathy (purpuric rash) Coagulopathy occurs early in patients with septicaemia. The laboratory findings of disseminated intravascular coagulation (DIC) are common in such patients. Coagulopathy is generally associated with the presence of a purpuric rash, but significant coagulopathy may infrequently occur in the absence of purpura. |
Renal failure Little or no urine output (<1ml/kg/hour) is a very early sign in septic shock, initially due to hypovolaemia. If shock persists then renal failure may occur. Serum creatinine  2 times upper limit of normal for age or 2-fold increase in baseline creatinine indicates renal dysfunction. 2 times upper limit of normal for age or 2-fold increase in baseline creatinine indicates renal dysfunction. |
Clinical pathophysiology of meningitis
Meningococcal meningitis generally has a better prognosis than septicaemia. Meningococci reach the brain from the bloodstream, implying that the patient’s immune response has prevented bacterial proliferation in the blood and not suffered overwhelming sepsis. This is because organisms are handled differently in these patients, which is probably due to differences in their inflammatory response to infection as well as different bacterial characteristics.
Deaths do occur, however due to the severity of the inflammatory process within the brain.
Once bacteria penetrate the blood-brain barrier, endotoxin and inflammatory mediators initiate a CSF inflammatory response, causing leakage of protein and fluid out of the cerebral vasculature. In addition, the processes delineated in septicaemia occur in brain blood vessels, causing cerebral oedema and cerebral vascular thrombosis. As a consequence there is an increase in brain water content and an increase in intracranial pressure. Both the increased pressure and thrombosis may lead to a reduction in cerebral perfusion, and consequently cerebral infarction and sometimes brain death.











